Invented in 1974 by a Chinese physician, the no scalpel vasectomy is becoming the most popular method of birth control in the United States.
This following is essential information about your procedure. This should not be thought of as optional. You need to know this. The reader is encouraged to search for similar topics on their own if they would like more information. I have eliminated all references from these pages as sites change too rapidly and previous working links become unusable too quickly.
A brief overview
Please wear a T‐shirt to the procedure, and bring tight-fitting underwear like tighty-whiteys. After a brief blood pressure and mini‐check‐up, I’ll use an elastic band to hold your penis to your shirt, and then cleanse the entire area with Betadine. A sterile drape is then placed over the site. The right vas is located and moved to the center of the scrotum. The skin is numbed with a small injection. Each vas is then numbed. Each of these injections takes about 10 seconds. Within 1 minute, you should be pain‐free.
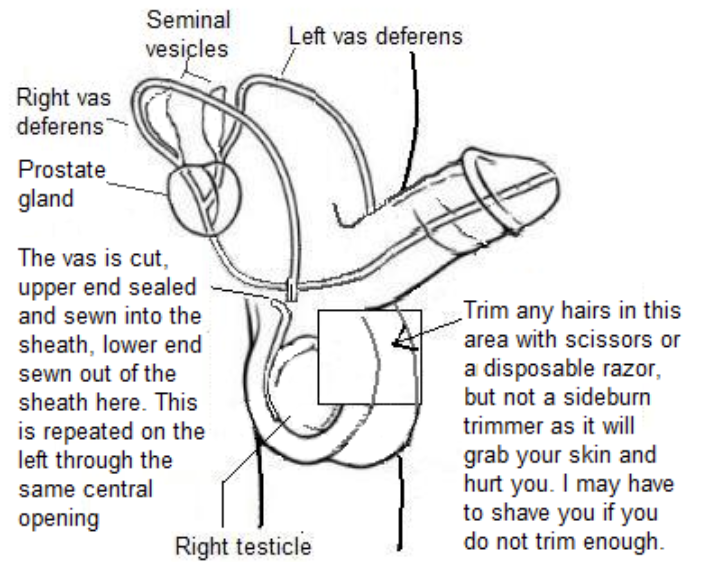
The right vas is then held still with a special clamp and the skin is opened with a special forceps. This forceps is then used to remove the sheath from the vas, and the vas is blocked with a short scar inside the upper piece. The upper and lower sections of the vas are then separated with a scissors and the upper vas is sutured inside the sheath with dissolving suture. The lower vas is sutured outside the sheath. The left side is then done identically. Note that this is called an open‐ended vasectomy. No stitches are necessary to close the skin opening. Operating time, start to finish, is usually 10‐15 minutes. You should be out our door within a half‐hour of entering it.
What’s to fear?
The minor complications possible are generally short‐lived and resolve with ice, rest, anti‐inflammatory medication, and time. Long‐term safety with NSV is considered excellent, although all of the following are possible:
Bruising: This is almost 100% going to happen. Sometimes it is quite colorful. It is harmless and goes away with no treatment.
Mild discomfort: Some men report a mild aching sensation to the scrotum for a few hours to a few days after the procedure. Rarely this lasts
longer.
Mild Bleeding into the scrotum (1/400): This may form a small tender swelling for a few days.
Scrotal Hematoma (1/1000): A major bleed into the scrotum causing a grapefruit‐sized tender scrotum which may take months to heal.
Infection (1/100): May present as redness and tenderness at the healing site opening or non specific tenderness within the scrotum, which may require oral antibiotics. More serious infection is possible, i.e. abscess formation, which may require intravenous antibiotics (1/1000).
Epididymitis (1/100): Tender swelling of the epididymis, the tube connecting the vas deferens and the testicle.
Sperm granuloma (1/500): A small, potentially uncomfortable, bead‐like structure made of leaked sperm that may develop at the site where the tube was cut and blocked if a traditional (as opposed to an open‐ended) vasectomy is chosen.
Post Vasectomy Pain Syndrome (1/1000): A rare complication of a persisting dull ache in the testicle where the inflammation does not settle down. It may resolve on its own or may need another surgical procedure.
Failure (less than 0.1%): Because a doctor has inadequately blocked one or both tubes, or because one (or both) tubes has rejoined.
Other uncommon complications have been reported.
I recommend a thorough web search for vasectomy information and side effects. Some sites are more reliable and others are just blog sites where unhappy people are very vocal. I recommend Mayo Clinic and Cleveland Clinic sites in the USA, and the Pollock Clinic site if you are from Canada. Telling patients about one thing that happened once with clips is not pertinent when I do not use clips at all.
Why an open-ended No-Scalpel Vasectomy?
A scalpel vasectomy takes twice the time and bleeds more, as it uses two incisions. Traditional vasectomy closes both ends of the vas, causing increased testicle pressure. With no closed testicular end, the open‐ended version reduces pain.
What about my sex life?
Your sex drive should not be bothered by a vasectomy. You will still have orgasms, and you will still have semen come out when you do. It just won’t contain sperm. Sperm usually makes up about 3% of semen.
How effective is it?
It is over 99.9% effective at preventing pregnancy. That makes it more effective than any other permanent method except abstinence.
Can it be reversed later?
It can be done, but fertility rates diminish as the years pass. Don’t have one if you are not sure. Reversal is very expensive and insurance will not cover it.
What other options are there for birth control?
Please do a quick Internet search for Birth Control Options.
- Compared to tubal ligation, vasectomy is much less invasive, does not increase PMS, and has a 3.33 times lower failure rate.
- The Essure fallopian tube implant and the hysterosalpingogram to prove it worked are expensive and painful.
- The IUD (intrauterine device) is less effective and increases the risk of pelvic infections.
- Birth control pills have nearly the same effectiveness as vasectomy, but are far more expensive, and are hormonal, as is the NuvaRing or the Implanon device.
- Condoms and foam together have a 0.3 to 4.5% failure rate but are inconvenient and costly. Either one alone is far less effective.
- A diaphragm is less effective and brings an increased risk of urinary tract infection.
- Withdrawal before climax is very ineffective and those who try this are usually called “parents.”
For all these reasons, it’s my feeling that men who have vasectomies are picking the easiest and least expensive permanent birth control option.
How do I prepare?
The week before: Avoid aspirin or any anti‐inflammatory pills for one week before the procedure. It’s smart to save alcohol consumption for afterwards, too. All of these increase bleeding. Use of Tylenol or generic acetaminophen is safe. If you are a very nervous person, call us for an anti‐anxiety prescription if desired.
An hour before your vasectomy: Use antibacterial soap and water to wash your penis and scrotum. Trim the hair in a two by two‐inch path down the front of the scrotum starting at the base of the penis. Please make sure no hairs can even stretch into this area. Your procedure time can easily double if I have to shave you. Shave as shown in the drawing below:
Bring a fresh pair of tight fitting jockey‐type underwear or jock strap to the procedure. This will help to keep your scrotum still. No boxer shorts, please. Feel free to bring an MP3 player to occupy your mind.
What about afterwards?
Here are the aftercare instructions that you will receive as you leave the office that day. It is important that you follow these instructions.
- Tonight, go home and gently remove the Betadine with a washcloth everywhere except right at the surgical site. Apply triple-antibiotic ointment or Vaseline to your gauze and let it fall back on the vasectomy site. Repeat this after each shower/bath. Wear the gauze and jockey shorts until your skin is healed. Do not push ointment into the opening of the surgery site. Just smear it on the gauze.
- Sit still and do next to nothing for two days. No fishing, horseshoes, skiing, skating, golfing, or anything more strenuous than watching TV. You should move only from the bed to the couch to the table and to the bathroom. Sex may be resumed in one week.
- Place ice on your scrotum to reduce bleeding, swelling, and pain, for 20 minutes every one to four hours, depending on pain intensity. “Gel Packs” intended to be kept in your freezer in the event of a sprain or zip-lock bags filled with ice work well.
- Take Aleve liquid gels 1-2 twice a day with food or Ibuprofen 200mg three to four at once three times a day with food for seven days to reduce pain (unless you are allergic or cannot tolerate it). Call me in the extremely rare event this is not enough help for your pain.
- Wear snug fitting jockey shorts (not boxers) for 3-4 days, 24 hours a day. These will also hold the 3″ x 3″ gauze squares against your skin like a bandage, in case there should be any slight leakage of blood. Replace these as needed until all staining of the squares stops (usually 2-3 days). You may shower or bathe 24 hours after your procedure, not before. For the first several days, do not spray a hand-held shower nozzle directly at your scrotum: this could force water through your vasectomy site and into your skin. Just let it trickle down your skin from above.
- You must prove that this was an effective surgery! There is no extra charge to prove this if you reside locally. After at least 20 ejaculations, or 3 months, whichever comes first, TEXT or call me at 269-615-3423 and we will decide on a Friday evening for you to bring your sample back to this location. Call Jan at 269-580-2340 when you arrive, and she or I will take your sample from you at your car window. I will look at your specimen, and report the results to you by 7 PM most often if I get it at 6:30 PM. Do not refrigerate the specimen, it must be fresh within two to three hours. I will need to see no sperm at all or 0-2 per high power field, non-moving (dead) sperm under the microscope. If there is anything else, you will be asked to repeat the sample after 10 more ejaculations.
- If you turn in a sample before 3 months, please repeat a post-vas semen check 3 months after the first successful one to ensure that the vas ends are not managing to grow back together. A second plastic container is in your take-home bag for this purpose, but if you have misplaced it a ziplock bag will work fine.
I look forward to providing your no-scalpel vasectomy. If you have any concerns or questions about this, please call me.
Kurt P. Helgerson, MD
If you do not find the answers to your questions above, please send me an e-mail and I will do my best to respond to you promptly.
